The speed at which new healthcare technologies are emerging is unprecedented. Some bring significant health improvements for previously intractable conditions, while others offer modest clinical benefits. These innovations put pressure on budgets everywhere, and although this is politically difficult to accept, it is a fact that no country, no matter how wealthy, can fund all the therapies and treatments that all people need. Choosing to fund some services necessarily means not funding others, and these decisions have consequences for the population’s health.
Technically, this is known as the opportunity cost: the benefit we could have received but which we forgo by taking another course of action. What is the opportunity cost of financing high-cost drugs in low- and middle-income countries? Should opportunity cost be factored into the decision-making process?
The Opportunity Cost of Financing High-Cost Drugs: The Case of Colombia
A recent study published by the Inter-American Development Bank in 2023 estimated how much health is gained or lost in Colombia by financing 10 high-cost drugs, selected based on their budgetary impact and annual cost per patient and/or treatment.
Colombians have access to a wide range of health services through an explicit benefit program provided by the national insurance system. They can also obtain treatments not included in that package through special requests from the treating physician or a court order.
Through the official information on the treatments not included in the health benefits plan, the authors calculated the opportunity cost of 10 drugs among those with the highest cost per patient and/or with the greatest impact on the health budget.
The selected drugs treat orphan diseases, autoimmune or degenerative disorders, cancers and diabetes. Annually, they benefit 23,261 patients at a cost per patient of between US$614 and US$179,000. To quantify the opportunity cost of these drugs, the authors calculate their Net Health Benefits (NHB).
Roughly speaking, the NHB is the additional health provided by the high-cost drug compared to the alternative, minus the health that can be achieved if the additional resources needed to finance that high-cost drug were used instead to improve the timeliness of and access to other services throughout the health system.
The results show that the 10 high-cost drugs provide additional benefits ranging from two weeks to a year and a half of living in perfect health throughout treatment, with a cumulative cost to the health care system of $543.5 million over the course of treatment for all those receiving them. If these resources were invested in the health system as a whole, the Colombian population would gain 88,000 years of life in perfect health.
Analyzing the Costs and Impact of Medications
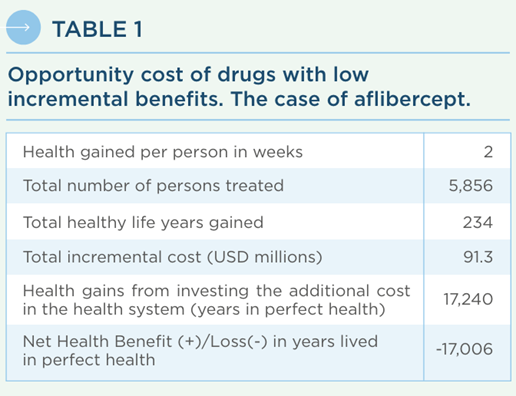
Other interesting results emerge from the study. Contrary to what might be expected, the drugs with the highest prices do not always have the highest opportunity costs. An example is aflibercept, for macular degeneration, which is priced at US$2,100 per year per patient: given its limited additional benefit and the number of patients receiving it, it has the second highest opportunity cost of 17,000 life-years in perfect health (see Table 1). That is, even moderately priced drugs can have significant opportunity costs if their clinical benefits are limited and if they are prescribed for a large number of patients.
Another interesting result is that, although higher prices on average are associated with higher health gains, this relationship is tenuous at best. For example, both nusinersen for spinal muscular atrophy and abatacept for rheumatoid arthritis provide an additional 1.4 years in perfect health compared to alternative treatments; but the former at an additional cost of US$1.5 million during treatment versus just US$24,000 for the latter.
Finally, some high-cost drugs have a high variability of market prices. This affects the opportunity cost and may even make the high-cost drug a better alternative. An example is lenalidomide, for certain cases of leukemia. For the initial estimation, average market prices were used for both lenalidomide and its comparator (bortezomib). But using the lowest prices among those reported for both drugs, lenalidomide was found to be more effective and less expensive, with a net benefit of 376 healthy years.
The decision-making process must incorporate issues beyond efficiency, including equity and prioritization of those who suffer the most. However, these results illustrate that decisions have costs in terms of gains and losses in lives and quality of life. Therefore, countries seeking to improve population health should include opportunity costs in decision-making to align policies accordingly.
Economic evaluations can help make informed decisions by making opportunity costs explicit, and countries can adopt a wide range of policies to minimize the opportunity cost of high-cost medicines.
We invite you to read more about this topic in our technical note: What is the opportunity cost of financing high-cost medicines: the case of Colombia (available in Spanish). You can also access tools and strategies for more efficient health spending in Smart Spending for Health: How to Make Each Dollar Count.


Leave a Reply