Addressing the large and growing burden of non-communicable diseases in the Latin American and Caribbean (LAC) region requires better prevention and screening but also improving diagnosis, treatment, and control of the conditions once they have developed. This needs concerted action by health systems, healthcare providers and patients, as well as other stakeholders – such as the food and beverages industry and society overall – to reduce both the disease incidence and long-term management.
A large and growing drag on health and resources
Among all non-communicable conditions, chronic cardiometabolic diseases (CMDs) are a particularly urgent concern in LAC because of their disease burden and economic impact. The two leading groups of CMDs, cardiovascular diseases and diabetes mellitus, rank first and third by their contribution to the burden of disease (see table). Together they represent more than 20 per cent of the total disease burden and more than two-thirds of deaths in the region. CMDs are also a major driver of rising health expenditures in the region. What is more, the main risk factors for these conditions – such as increased blood pressure, high blood sugar and cholesterol, and excess weight – remain prevalent and are generally increasing in LAC.
Top-3 conditions according to their disease burden in LAC in 2019
| Disease burden* | Share of total disease burden | Deaths | Share of deaths | |
| Cardiovascular diseases | 20.4 million | 12.3 % | 962 thousand | 26.9 % |
| Cancers | 16.5 million | 9.9 % | 638 thousand | 17.8 % |
| Diabetes and kidney diseases | 13.7 million | 8.3 % | 395 thousand | 11.0 % |
Persistent and large gaps in CMD treatment and control
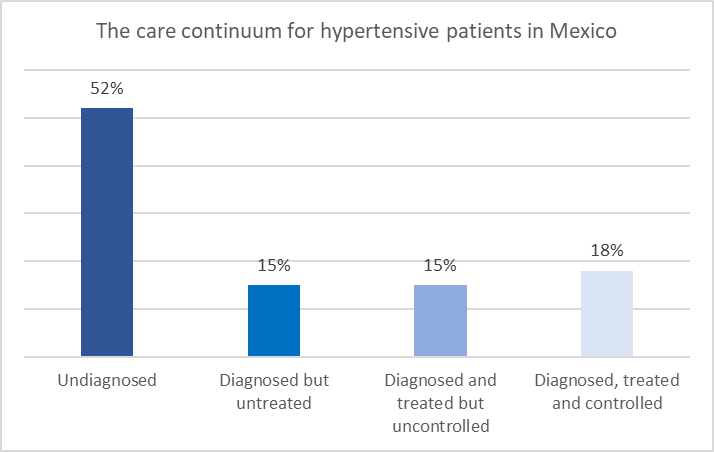
In addition to prevention, it is critical for LAC countries to effectively diagnose and manage CMDs once they have developed. One way to understand this is the “care cascade” that describes the stages in the sequence from the initial diagnosis of a condition to treatment and ultimately achieving control. There are substantial problems at each stage. The below graph shows this using data from recent analysis in Mexico:
- 52% of patients with hypertension are undiagnosed.
- 15% of these patients are diagnosed but do not receive treatment.
- 15% receive treatment but have uncontrolled hypertension.
- Only 18% have controlled hypertension.
There are similar challenges for other conditions and countries. For example, fewer than two-thirds of Colombian patients diagnosed with diabetes mellitus had a recent blood sugar report and only about half of these had achieved glycemic control.
Too many patients are stuck or regress
Over time, many patients who have been diagnosed do not advance or even regress toward lower stages of the care cascade. The aforementioned Mexican study followed survey participants who had high blood pressure in 2005/6 and examined their status checked several years later, between 2009 and 2012. The below table shows the key findings:
- Many patients are stuck in lower stages of the care continuum (the yellow cells). For example, 70% of those diagnosed but untreated at baseline remained untreated a few years later.
- Few patients advance in the cascade (the green cells). For example, only 25% of those who were treated but had uncontrolled hypertension at baseline had achieved control at the time of the endline.
- Many patients regress toward earlier stages of the cascade (the red cells). 40% of controlled hypertension in 2005 dropped out of treatment entirely by the endline while only fewer than a quarter (23%) maintained control.
So just getting patients to one of stages in the care cascade is not at all sufficient: we also need to make sure that they do not regress and instead advance to later cascade stages.
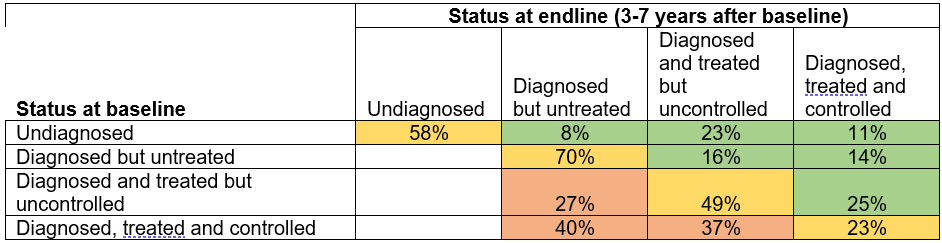
Source: Based on study by Mauer et al. 2022; data for Mexico 2005/6 (baseline) to 2009/12 (endline).
Evidence-based solutions are available but concerted action is needed
Overall, this means that countries need to urgently improve screening and diagnosis, but also better manage CMDs once they have been diagnosed – along all stages of the cascade. The good news is that there are interventions and policies to improve the care cascade. They range from better primary care and access to essential medicines, to telemedicine and digital tools, and to nudges for providers and patients.
The main challenge is to get all stakeholders on board and align their efforts for maximum impact, and to reimagine and restructure how each stage of the care cascade is addressed. The health system needs to provide an enabling structure that champions chronic disease care, health care providers need to have the right incentives and resources to encourage consistent accessible and high-quality care, and patients need to be active participants. To tackle the CMD epidemic, focusing on a single stage in the cascade will not be effective, and we need concerted and purposeful action on all fronts.


Leave a Reply