Countries in Latin America and the Caribbean (LAC) face major challenges in meeting the demand for available personnel with the medical skills needed to care for the population. In this context, what is possible and what is desirable for future healthcare workers? And how do we prepare to shape the skills and functions required for the coming decades?
The Inter-American Development Bank (IDB) publication Toward the Future of Healthcare Workers: upcoming trends and challenges addresses these questions. In this blog, we highlight the main findings.
The Importance of Healthcare Workers: Today and in the Future
Healthcare workers are the backbone of healthcare, withtheir main goal to improve the health of individuals and populations. It is essential to understand the current context and create frameworks to establish the number, availability, distribution, training, skills and working conditions of future healthcare workers.
Healthcare workers currently face significant challenges. For example, greater efforts are needed in order for LAC countries to achieve universal health coverage. Gaps still exist in access to health services, which is partly due to the shortage of healthcare personnel.
In addition, the region’s adult population is aging and the proportion of people with chronic diseases is rising. On average, 10% of the population are over 60 years old; 60% are overweight or obese; 20% have high blood pressure; 9% have diabetes; 9.3% suffer from anxiety and 5.8% from depression. As a result, healthcare needs are complicated and will become more so in the future. Personnel with specific skills will be needed to care for older adults and patients with chronic diseases and mental health conditions.
The COVID-19 pandemic revealed the precariousness and lack of preparation of healthcare workers in managing public health emergencies and the gap in access to essential services grew wider. As a result, the population – as consumers of health services – expressed the need to be heard, to participate in decision-making regarding their health and for their preferences and rights to be recognized.
What Is the Situation of Healthcare Workers in the Region?
In order to have the necessary number of healthcare personnel and to provide optimal working conditions, multiple difficulties must be addressed, including:
- Health personnel are predominately female, and women face unfavorable working conditions, making it difficult to balance work and family roles. Women’s income is 30% lower than that of male colleagues, and they have fewer opportunities to hold managerial positions.
- LAC countries do not have sufficient healthcare personnel. On average, the region has 56 healthcare workers (doctors, nurses, midwives) per 100,000 inhabitants. Although this figure exceeds the WHO-recommended minimum of 44.5 per 100,000 inhabitants, in practice most countries still fail to reach this threshold.
- Having the required number of health personnel is necessary, but not enough, since distribution is inequitable — healthcare workers are scarce in rural areas and concentrated in urban areas.
- University training and continuing education are heterogeneous. Opportunities for undergraduate and graduate studies are limited in the region, and the shortage of investment, teachers and educational infrastructure limits expectations for achieving the required number of health personnel.
Innovations for Personnel in the Healthcare Field
Countries such as Argentina, Brazil, Chile, Colombia, Mexico, Peru and El Salvador have made significant progress in improving their policies to meet the demand for skilled healthcare workers.
Task shifting, for example, is a significant step forward. The tasks of one health professional are transferred to another with a lower or different level of training. Tasks are reconfigured to improve efficiency in management, correct imbalances in distribution and attain the necessary competencies. Nurses are the benchmark for task shifting since they are expanding their clinical activities and working at the interface between traditional nursing and the medical profession – diagnosing, prescribing and performing surgical procedures.
As a result, multiple profiles and disciplines exist among health personnel, such nurse practitioners, healthcare managers, care coordinators, and in the different branches of genetics and specialists in medical informatics.
Digital technology and healthcare services are converging and creating multiple profiles, mainly in clinical services, healthcare systems, project management, behavioral and organizational management, analysis and evaluation, data management and information technology. And the interaction between healthcare providers and patients is being digitalized in response to the demand for greater transparency, convenience, and access to personalized healthcare services.
The Future of Healthcare Workers
Future planning is needed to address the remaining challenges, and planning for health personnel must be a priority on the health-systems agenda.
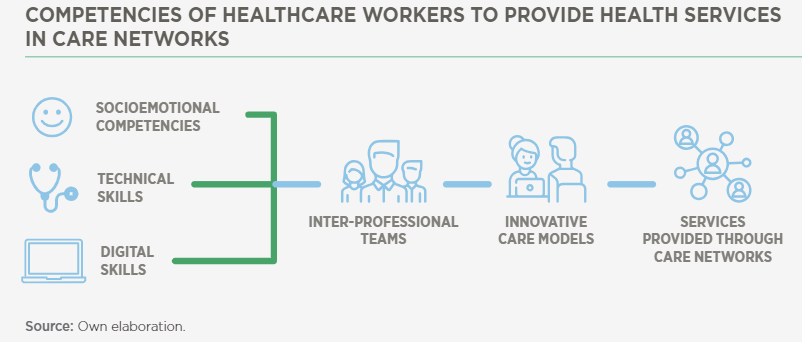
It is important for healthcare workers to develop multiple skills. For example, they must adapt to and work in a context of continuous technological innovation. Training in ethics is also essential, since medicine has always been at the intersection of science and society, and nowadays technology is advancing faster than ethical and legal standards. Advances in genetics, for example will pose new ethical dilemmas; the COVID-19 pandemic presented healthcare personnel with ethical problems arising from the rationing of care and the equitable allocation of resources. In this sense, the healthcare workforce will need to strengthen multiple socioemotional, technical and digital skills in a future with complex healthcare needs, constant technological change and innovation, and limited resources.
Health education must be expanded to include new professions consistent with market needs. For example, robotic engineering, data science and genomics will all be indispensable in the near future.
In addition:
- Technologically compatible healthcare environments will be created jointly among the different health / technology / digital disciplines along with the public’s participation.
- Technological changes will improve rather than replace the performance of healthcare workers.
- The workplace and patient care are definitively separated. Telehealth and telemedicine technology will transform work environments, allowing greater freedom with respect to the workplace and work hours of health personnel.
- Remote work, together with task shifting and skill mixing, will promote greater access to and flexibility in health services.
- Priorities on the health-services agenda will include participation of the health sector in mitigating its carbon footprint and training and care of healthcare personnel in the effects of climate change on the population’s health.
In conclusion, it is critical to identify what can and should be changed in the future. Educational institutions and health systems face the challenge of creating the conditions that will enable them to meet the demand for available personnel with optimal working conditions, who have the resources, skills and competencies to meet the needs of the population.


Leave a Reply