Type 2 diabetes affects millions of people in Latin America and represents one of the greatest challenges for health systems. In Ecuador, this condition particularly impacts rural and vulnerable populations, such as those in the province of Chimborazo, where health centers must respond to growing demand with limited resources.
To address this challenge, the Ecuadorian Ministry of Public Health, with support from the Inter-American Development Bank (IDB) and the Institute for Healthcare Improvement (IHI), implemented a pilot project that demonstrates that it is possible to improve chronic disease care by implementing quality improvement methods, strengthening local capacities, and using data more strategically.
In just seven months, this initiative achieved remarkable results in controlling type 2 diabetes, promoting a model that could be replicated in other regions of the country and in Latin America and the Caribbean.
A model based on continuous improvement and data use
The project was implemented in 11 primary and secondary health facilities in Chimborazo, where staff received intensive training in continuous improvement tools. The methodology was based on the Plan-Do-Study-Act cycle, which allows problems to be identified, solutions to be tested, and results to be measured.
The approach views health organizations as interdependent systems: improving processes requires understanding data variability, learning from practice, and promoting sustained changes in the behavior of the health team. With technical support, coaching, and learning sessions, the teams were able to identify obstacles in care, design solutions adapted to their reality, and implement them immediately.
Large gaps in diabetes control
As a baseline, between October and December 2024, the data showed gaps:
- Only 3% of people over 40 were screened for type 2 diabetes.
- Only 4% of diagnosed patients were evaluated for possible complications.
- None had scheduled follow-up appointments.
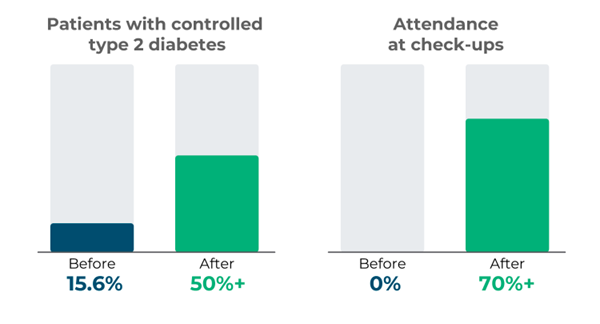
In addition, only 15.6% of patients had their disease under control, while a quarter already had complications such as diabetic foot, retinopathy, or kidney failure. These data prompted participating facilities to set concrete, measurable, and ambitious goals.
Better control and follow-up
Within seven months, the change was evident. Regular screening was implemented, follow-up appointments were scheduled, and an active search began for patients who were not attending their check-ups. Also, the early detection of complications was strengthened. The results:
- The percentage of patients with controlled type 2 diabetes rose from 15.6% to over 50%.
- Attendance at check-ups increased from 0% to over 70%.
All this was achieved thanks to local leadership, staff collaboration, and the intelligent use of data. By December 2025, the teams set out to achieve 70% screening in adults, get 50% of patients to keep their diabetes under control, and reduce the rate of complications.
The Chimborazo experience shows that improving primary care and chronic disease management does not always require more funding, but rather best practices, local leadership, and technical support.


Leave a Reply